Shoulder Dislocations & Instability
A board-certified, fellowship-trained orthopaedic shoulder surgeon and sports medicine specialist, Dr. Steven Chudik is renowned for his arthroscopic shoulder expertise and innovative procedures that reduce surgical trauma, speed recovery, and yield excellent outcomes.
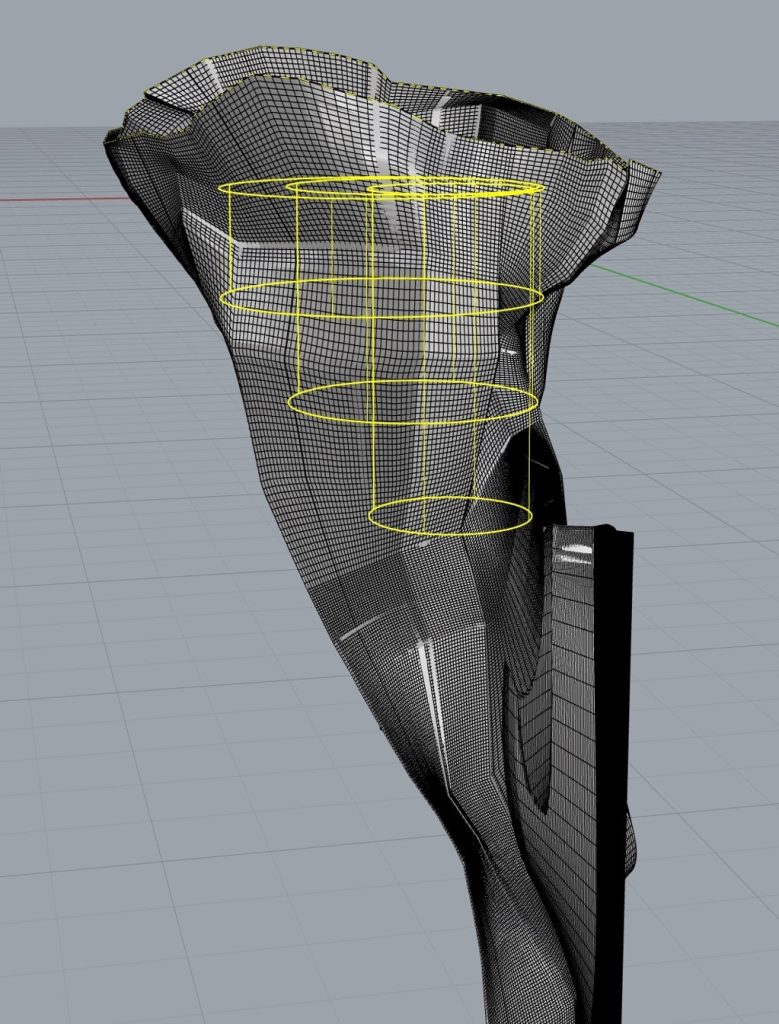
Through his research, Dr. Chudik investigates and pioneers advanced and novel arthroscopic procedures, instruments, and implants that have forever changed patients’ lives. Never content to settle for what’s always been done for orthopaedic shoulder care, Dr. Chudik prides himself on providing individualized care and developing a plan that is right for each patient. By taking this approach for the past 20 years, Dr. Chudik has developed minimally invasive surgical techniques, instruments, and implants for the arthroscopic repair of shoulder dislocations and instability. One that has changed countless patients’ lives for the better is an arthroscopic technique Dr. Chudik developed to rebuild a patient’s damaged glenoid (shoulder socket) caused by repeat shoulder dislocations.
Shoulder Instability Expertise
- Anterior Shoulder Joint Dislocations and Instability
- Posterior Shoulder Joint Dislocations and Instability
- Labral Tears (Bankart tears)
- Bony Bankart Injuries
- Multi-directional Shoulder Instability
- Bony Bankart Repair and Glenoid Reconstruction
- Internal Impingement and Microinstability
- Arthroscopic Hill-Sachs Fracture Repair and Remplissage Surgery
- Arthroscopic Capsular Tear Repair and Capsular Plication
- Arthroscopic Humeral Avulsion of the Glenohumeral Ligament (HAGL) Repair
- Superior Labral Tears (SLAP tears) and Repair
- Return to Sport Dynamic Shoulder Stability Training
- Return to Sport Testing

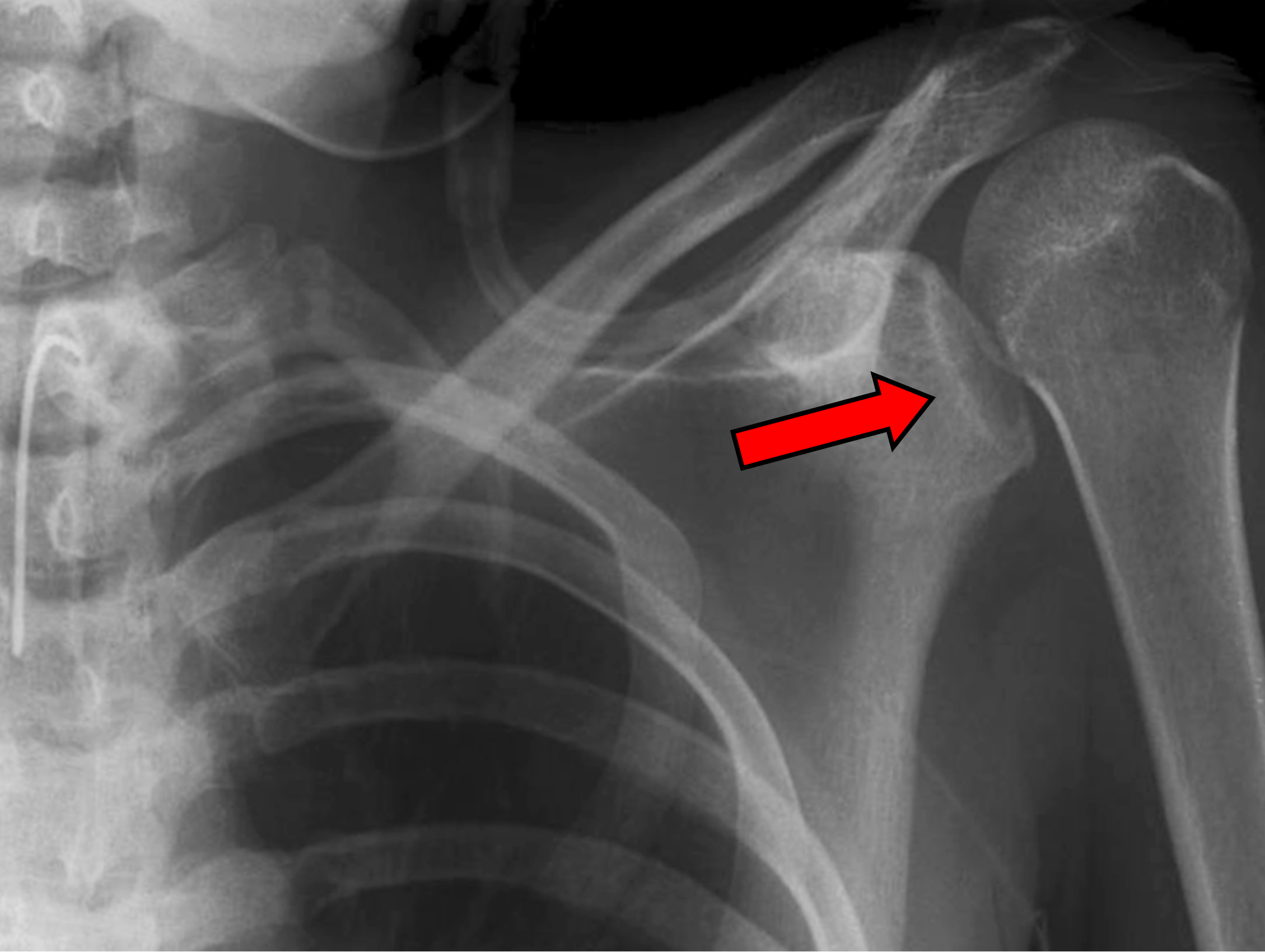
3-D CT scan shows glenoid bone loss of more than 20 percent from recurrent shoulder dislocations.
Individualized Treatment, Rehabilitation and Return to Sport Protocols and Testing
Because no two people and no two injuries are alike, Dr. Chudik uses his expertise to develop and provide individualized care and recovery plans for his patients. This personal attention explains why patients travel to have Dr. Chudik care for their shoulder conditions and injuries.
Dr. Chudik expects better than average outcomes and provides specific treatment, rehabilitation, and return to activity protocols for golf, throwing and other overhead sports, as well as return to sport testing. He also developed and researched an objective test protocol for determining when it is safe to return to sport following a shoulder dislocation and surgical repair.
Frequently Asked Questions
Answer to the Question
Testimonials and Patient Stories
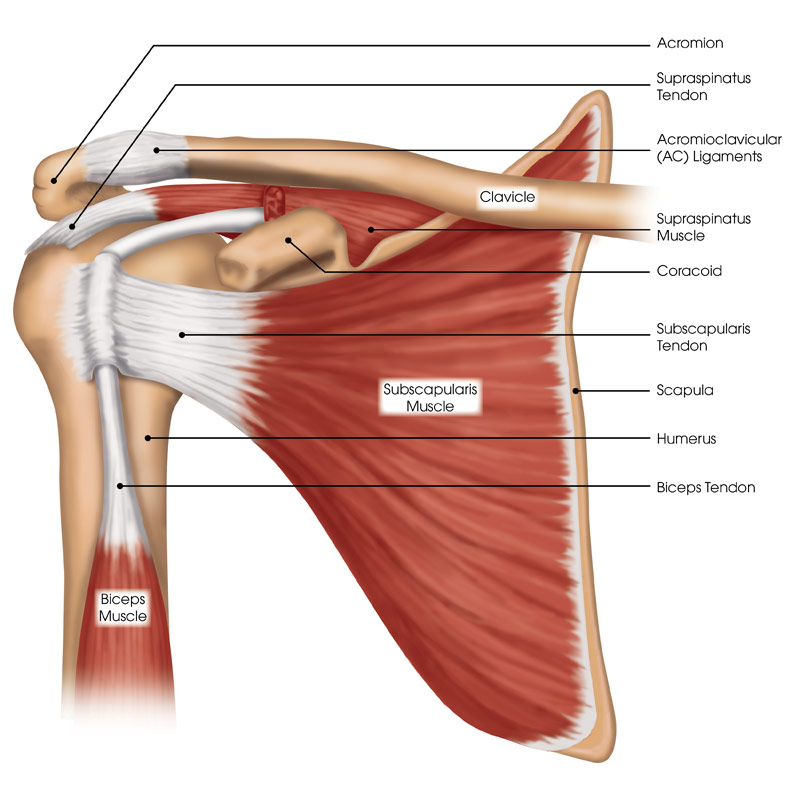
Shoulder Anatomy
The shoulder possesses a remarkable range of motion, making it one of the most mobile and important joints in your body. Whether you are throwing a baseball, working overhead, or performing everyday tasks of reaching and carrying, your shoulder motion and stability are critical to this high level of function. Unfortunately, this increased mobility and structural complexity makes your shoulders susceptible to injuries that can be quite limiting and disabling.
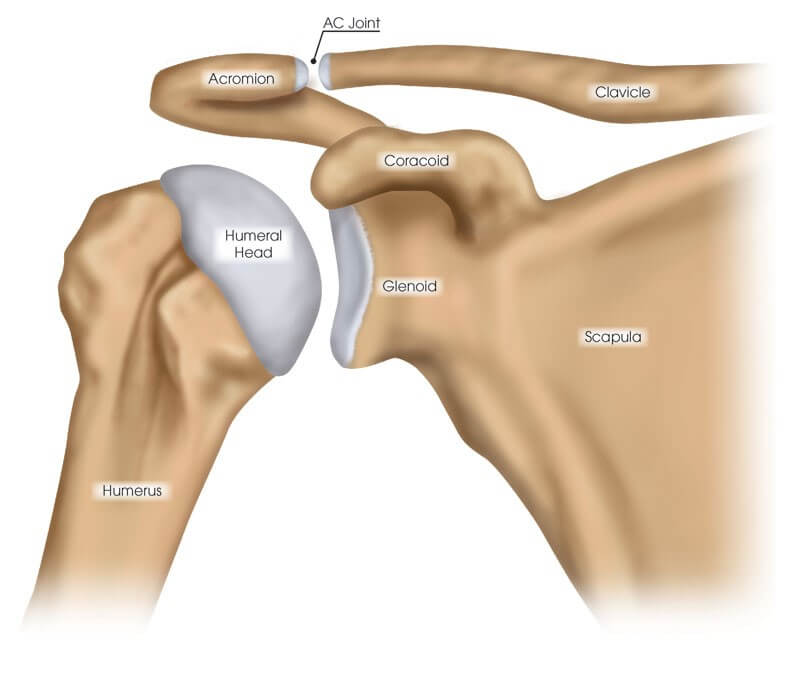
The shoulder consists of three bones, three main joints, and an articulation between the scapula (shoulder blade) and thorax (chest):
- Scapula (shoulder blade)
- Clavicle (collar bone)
- Humerus (upper arm bone)
- Glenohumeral joint (shoulder joint)
- Acromioclavicular joint (shoulder blade-collar bone joint)
- Sternoclavicular joint (sternum-collar bone joint)
- Scapulothoracic articulation (shoulder blade-chest connection)
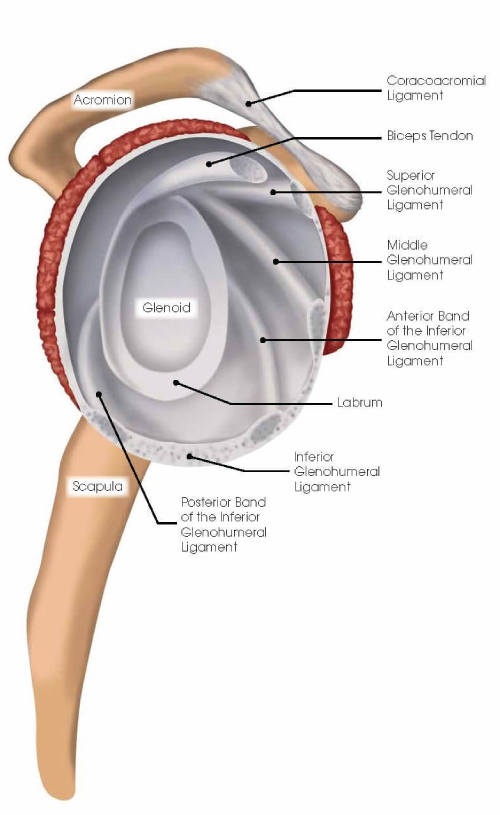
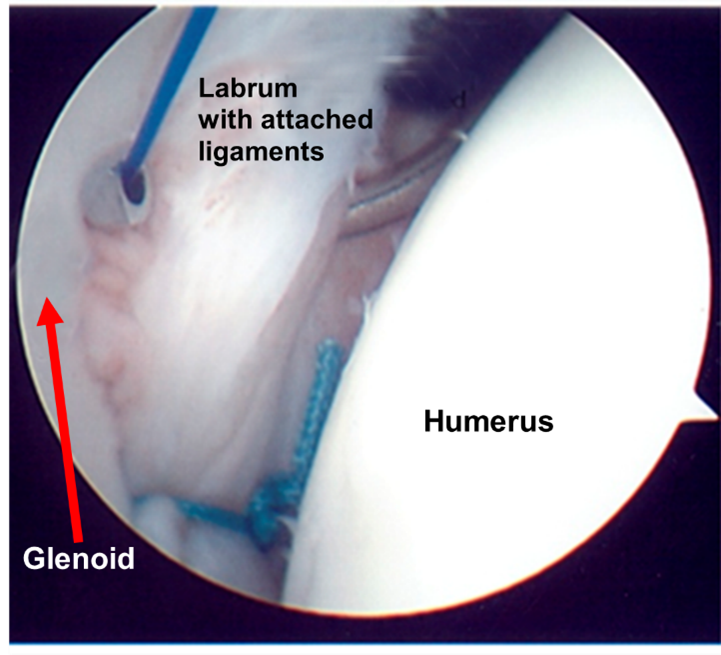
Labrum and Ligament Anatomy
The shoulder has a labrum or thickening of firm soft tissue attached to the rim of the glenoid (socket). It deepens the socket to increase stability, bears the load, and serves as the attachment point for ligaments that run between the upper arm bone and the bony glenoid (socket).
Ligaments are strong soft-tissue bands that connect bones at a joint and provide stability and proper limits to motion. The labrum and ligaments may be torn if forces cause the humeral head (ball) to abruptly shift from the glenoid (socket) such as during a shoulder dislocation. Shoulder ligaments get their names from the bones to which they connect and include the superior glenohumeral ligament (SGHL), middle glenohumeral ligament (MGHL), and the inferior glenohumeral ligament (IGHL) with important anterior and posterior bands. There also are other important ligaments in the shoulder including the acromioclavicular, coracoclavicular, and sternoclavicular ligaments.
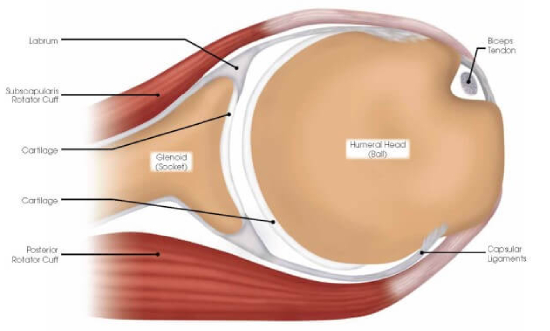
Cartilage
The joint surfaces of the shoulder are covered with a thin, but durable layer of cartilage over the ends of the humeral head (ball) and glenoid (socket) that allows the shoulder surfaces to articulate, and move smoothly—almost frictionless and painlessly along each other. The cartilage lacks a blood supply. It gets nutrition from the joint fluid. Without a blood supply and because of its relatively less active cellular makeup, cartilage does not maintain or repair itself. The cartilage is extremely durable, but in time with “wear and tear” or following injury, it breaks down, fails, and leads to cartilage damage and eventually symptomatic (pain, stiffness, swelling) arthritis (failure of this protective joint surface).
Muscles
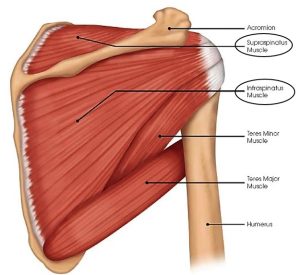
The shoulder has several muscles that help it move with proper coordination and strength to accomplish tasks ranging from simple reaching to high level overhead athletic maneuvers. Muscles are like loaded active springs. They attach to bones across joints by different shaped rope- or band-like tendons to exert their action and cause movement. The rotator cuff is a deep, core group of four muscles. They keep the humeral head (ball) centered on the glenoid (socket) while the pectoralis major, deltoid, and latissimus dorsi (the big muscle movers of the arm) create pulling and pushing forces that would otherwise shift the humeral head out of the glenoid (socket). Even with simply reaching out and away from your body the rotator cuff must generate forces equal to almost 80 percent of your body weight to keep the humeral head centered in the glenoid. Still, greater forces are needed during overhead throwing or strenuous lifting movements. These tremendous forces can cause tears in the tendon portion of the rotator cuff and result in pain and arm/shoulder limitations. The long head of the biceps muscle that attaches to the top of the glenoid through the superior (top) labrum also can be injured and cause pain. Additionally, muscles control the scapula (shoulder blade) or base of the shoulder joint which can be affected by injury and overuse producing shoulder pain and limitations.
Shoulder Instability
Because the shoulder has more motion than any other large joint in the body, it is the most commonly dislocated large joint. There are many structures in the shoulder that have to work together to provide stability and keep the humeral head (ball) seated in the glenoid (socket). Shoulder instability occurs when the humeral head separates from the glenoid. This can be a very quick, partial separation (subluxation), or it can be a more significant condition where the ball and socket completely separate and can get stuck out of place in a dislocated position.
Injuries and Conditions
Surgical Procedures
- Bony Bankart Repair
- Bankart (Labrum) Repair – Anterior
- Bankart (Labrum) Repair – Posterior
- Arthroscopic Repair of Humeral Avulsion of the Glenohumeral Ligaments (HAGL)
- Arthroscopic Bony Bankart Fracture Repair and Reconstruction (Developed by Dr. Chudik)
- Arthroscopic Hills-Sachs “Remplissage” Repair
- Arthroscopic Capsular Tear Repair-Reconstruction
- Arthroscopic Pancapsular Plication Surgery for Multidirectional (MDI) Shoulder Instability
- Acromioclavicular (AC) Joint Separation Repair and Reconstruction (Developed by Dr. Chudik)
- Sternoclavicular Separation Repair and Reconstruction
- Superior Labrum (SLAP) Tear Repair
About Dr. Chudik

- Curriculum Vitae (CV)
- Video
- Website: stevenchudikmd.com
- Schedule an appointment online
- Email: contactus@chudikmd.com
- Phone: 630-324-0402
Innovations

Through his research, Dr. Chudik investigates and pioneers advanced and novel arthroscopic procedures, instruments, and grafts that change patients’ lives because of better long-term outcomes, or outcomes that previously were never possible. His efforts continue to yield patent applications and patents that will positively affect orthopaedic surgical techniques worldwide.
Novel Procedures
US Patents and Patent Applications
Dr. Steven Chudik continually innovates to create new technology surgical techniques and improve patient care. He also collaborates worldwide with other leaders in the orthopaedic technology industry. Surgeries provide Dr. Chudik with an endless source of ideas to create new, safer, less invasive, and more effective surgical procedures, surgical instruments, and implants. Several of his patents are the direct result of these pioneering endeavors.
- Method of Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,445,910, filed September 11, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery. Patent application serial number 11/529,185 case II, filed September 25, 2006
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery, U.S. Patent No. 9,974,658, filed September 25, 2006
- Humeral Implant for Minimally Invasive Shoulder Replacement Surgery, Serial No.11/525,629, filed September 25, 2006, application published as U.S. Patent App. Pub. 2007/0016305 (A)
- Guide for Shoulder Surgery, U.S. Patent No. 9,968,459, filed September 29, 2006
- Suture Pin Device. Patent application serial number 11/529,2006, case XV, filed September 29, 2006
- Suture Pin Device, Serial No. 11/529,185, filed September 29, 2006, application published as U.S. Patent App. Pub. 2007/0027477 (A)
- Method of Arthroscopic or Open Rotator Cuff Repair Using An Insertional Guide For Delivering a Suture Pin, U.S. Patent No. 8,540,737, filed October 24, 2006
- Acromioclavicular Joint Repair System, U.S. Patent No. 9,387,011, filed February 2, 2007
- Resurfacing Implant for a Humeral Head, Serial No. 13/068,309, filed May 9, 2011, application published as U.S. Patent App. Pub. 2012/0041563 (A)
- Universal Anterior Cruciate Ligament Repair and Reconstruction System(Cannulated Scalpel), U.S. Patent No. 10,034,674, filed February 2, 2007
- Resurfacing Implant for a Humeral Head. Patent application serial number 13/068,309 case II (A), filed May 9, 2011
- Method of Arthroscopic or Open Rotator Cuff Repair Using an Insertional Guide for Delivering a Suture Pin. U.S. Patent Number 8,540,737 B2, issued September 24, 2013
- Cortical Loop Fixation System for Ligament and Tendon Reconstruction, Serial No. 13/998,567, filed November 12, 2013, application published as U.S. Patent App. Pub. 2015/0134060 (A)
- Acromioclavicular Joint Repair System. U.S. Patent Number 9,387,011 B2, issued July 12, 2016
- Method of Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,445,910 B2, issued September 20, 2016
- Guide for Shoulder Surgery. U.S. Patent Number 9,968,459 B2, issued May 15, 2018
- Glenoid Implant for Minimally Invasive Shoulder Replacement Surgery. U.S. Patent Number 9,974,658 B2, issued May 22, 2018
- Glenoid Implant with Replaceable Articulating Portion, U.S. Patent No. 11,406,505, filed August 20, 2019, issued August 9, 2022
- Cortical Loop Fixation Method for Ligament and Bone Reconstruction, Serial No. 15/731,719, filed July 24, 2017, application published as U.S. Patent App. Pub. 2019/0021845
- Humeral Implant and Method, Serial No. 17/532,714, filed November 22, 2021, published as U.S. Patent App. Pub. US 2023/0157832
- Humeral Implant with Cannulation and Method, Serial No. 18/211,396, filed June 19, 2023
- Glenoid implant with Portal and Method, filed July 2023
Dr. Steven Chudik continually innovates to create new technology, and surgical techniques and improve patient care. He also collaborates worldwide with other leaders in the orthopaedic technology industry. Surgeries provide Dr. Chudik with an endless source of ideas to create new, safer, less invasive, and more effective surgical procedures, surgical instruments, and implants. Several of his shoulder patents are the direct result of these pioneering endeavors.
Research
An inquisitive nature was the impetus for Dr. Steven Chudik’s career as a fellowship-trained and board-certified orthopaedic surgeon, sports medicine physician, and arthroscopic pioneer for shoulder injuries. It also led him to design and patent special arthroscopic surgical procedures and instruments and create the Orthopaedic Surgery and Sports Medicine Teaching and Research Foundation (OTRF). Through OTRF, Dr. Chudik conducts unbiased orthopaedic research, provides up-to-date medical information to help prevent sports injuries and shares his expertise and passion for mentoring medical students in an honors research program, and serves as a consultant and advisor for other orthopaedic physicians and industry research.